Talosnation
Whenever we talk about insurance and RPA automation, we can never skip ahead on claims. This is one of the highly critical departments of an insurance provider, which, when inefficient, would highly affect both the insurer and the insured.
Humans are great at thinking creatively and solving problems, but they aren't as good at repeating the same task over and over. When we ask them to repeat the same task again and again, it can lead to mistakes. Since claims management follows a step-by-step process, it's better to let people do what they do best and have RPA robots handle the repetitive tasks. Not sure what RPA is? Click here to learn more.
So, we're looking at how much of the work in a department can be automated to make things easier for people and reduce mistakes. From our research, we found that around 70% of the tasks can be handled by RPA, letting humans focus on the other 30%.
Now, let's dive into how this works. First, we need to understand the current workflow and identify the problems. Then, we can see how RPA can help fix them.
Let's walk through an example to see how the process works:
Imagine John is riding his bike on the highway and gets into an accident. Luckily, he's okay, but his bike is badly damaged. Thankfully, he has good motor insurance. Now, let's see what happens when he tries to claim insurance for his bike.
John's Journey: Navigating the Claim Processing Workflow for Motor Claim
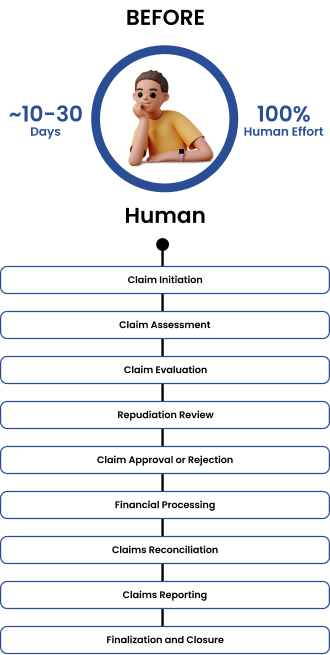
1. Claim Initiation
- Policyholder Report: John quickly tells his insurance company about the motor accident.
- Registration: The claim is speedily logged into the system, starting the process, and John is given a claim number.
2. Claim Assessment
- Initial Review: A claims adjuster quickly checks John's claim to make sure his insurance covers it and that all the basic information from John is correct.
- Documentation Collection: John provides necessary documents like reports, repair estimates, photos, and police reports. These are collected to process and evaluate his claim.
3. Claim Evaluation
- Detailed Investigation: After John's claim is registered, a claims adjuster conducts a thorough investigation into the accident, examining all the details.
- Damage/Loss Assessment: The claims adjuster carefully assesses the extent of damage or loss from the accident to determine the exact amount needed for John's claim.
4. Repudiation Review
- Review: This step is super important because it helps the insurer make sure John's claim is all good and doesn't break any rules. The insurer looks at everything really closely to check for any funny business or rule-breaking. Using AI or automated platforms here would be great because they're like super-powered detectives—they can handle lots of information quickly and help match things up for better fraud detection.
- Repudiation Notification: If the insurer can't approve John's claim, they let him know right away and explain why, so he understands.
5. Claim Approval or Rejection
- Review and Decision: Senior folks called adjusters or claims managers to take a good look at John's claim and make a decision.
- Authorization: After looking at everything, they decide if John's claim should get paid or not.
- Rejection Reasons: If they don't approve John's claim, they tell him why, so everything's clear.
6. Financial Processing
- Entry: The insurer accurately enters all of John's claim details into the accounting system for further processing.
- Reserve Management: The insurer sets aside enough money to cover John's claim and any others that have been approved.
- Payment Processing: Once everything's sorted, the insurer ensures timely disbursal of funds to cover John's damages.
7. Claims Reconciliation
- Ledger Updates: The insurer keeps track of changes in claims payments and reserves in the general ledger.
- Bank Reconciliation: The insurer matches payment transactions to make sure everything adds up correctly.
8. Claims Reporting
- Internal Reporting: The insurer creates detailed reports internally to summarize what's been happening with John's claim and manage reserves effectively.
- Regulatory Reporting: The insurer also makes sure to report everything to the right regulatory bodies to follow all the rules.
9. Finalization and Closure
- Claim Closure: When everything's finished, the insurer officially closes John's claim in their system.
- Document Archiving: The insurer carefully saves all the papers about John's claim for later checking.
The main issue with the current claim processing is dealing with lots of data for each claim. This makes things slow and sluggish. But with RPA and AI, things could be sped up a lot and be more accurate.
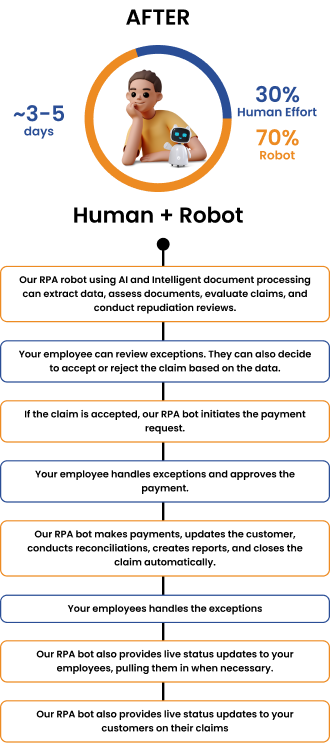
1. Claims Initiation
- Problem: Manual entry of claim details increases the risk of errors due to the repetitive nature of the task.
- Automation Opportunity: Use our RPA bots to automate your data entry, reducing manual effort and improving process efficiency.
2. Claim Assessment
- Problem: Document processing for claim assessment is tedious, leading to delays and potential errors.
- Automation Opportunity: Use our RPA bots to streamline your assessment process by extracting and validating data from various documents, such as accident reports and policy information, improving accuracy and efficiency.
3. Claim Evaluation
- Problem: It takes a long time to check policy terms, accident information, and documents for claim approval. Generali Insurance, a big insurance company, saved lots of money by using RPA everywhere—over 80 million USD. They even made a special RPA bot to check photos in claims.
- Automation Opportunity: You can use our RPA bots to help analyze your claim data and find patterns. This lets your claim adjusters focus on the hard stuff that needs human thinking. And if you bring AI into it, even more can be done.
4. Repudiation Review
- Problem: Checking claims for fraud or policy violations takes a lot of time and effort.
- Automation Opportunity: Use our RPA bots to spot any suspicious claims by looking at patterns and comparing data. This can help you find fraudulent claims faster, so your experts can focus on making important decisions. You can also improve the process with AI, which many companies are using to catch fraud better.
5. Claim Approval or Rejection
- Problem: It takes a lot of time to match claims with policy terms, which slows down decision-making.
- Automation Opportunity: You can speed things up by using our RPA bots to handle routine approvals. Your human adjusters can then focus on the tricky cases, making sure they fit the rules and regulations.
6. Financial Processing
- Problem: Entering claim details and processing payments manually can cause mistakes and delays.
- Automation Opportunity: Let our RPA bots handle tasks like data entry, managing reserves, and processing payments. This frees up your team to focus on making important financial decisions.
7. Claims Reconciliation
- Problem: It takes a lot of time for your employees to match up a claim's payments with financial records.
- Automation Opportunity: Use our RPA bots to automate this task. It'll save time and make sure your financial reports are more accurate.
8. Claims Reporting
- Problem: Your employees have to make reports by hand, which could cause delays and problems with following the rules.
- Automation Opportunity: Use our RPA bots to make reports automatically. This will give your employees more time to think about big decisions and make sure the reports are always on time and correct.
9. Finalization and Closure
- Problem: It takes a lot of time for your team to finish paperwork and store documents for closed claims.
- Automation Opportunity: Let our RPA bot handle closing claims and organizing documents. This way, your team can focus on solving tough claims and giving great service to customers.
10. Live Status Updates
- RPA can do more than just manage claims. It can watch over the whole process and keep humans in the loop when needed. Plus, it can update customers on their claims, making them happier and reducing the work for your customer care team.
11. RPA + API
- The current workflow was made with humans in mind. They could only see, read, enter, or copy-paste information. But with RPA, we can use APIs to let systems and robots talk to each other. This makes things faster and more detailed.
So, there you have it – RPA to your rescue! By harnessing the power of automation, we can streamline your Patient Onboarding process, slash processing times, and free up your valuable time and resources for more strategic tasks.
While these areas give us a good idea of how RPA can boost efficiency and productivity, there might be even more opportunities when we zoom in and look at the finer details. Since all company's processes are unique, we can't give specific advice until we take a closer look at each one. If you're curious to learn more, don't hesitate to reach out to us at https://www.talosnation.com/contact or drop us a message on LinkedIn. We're always here to chat and help out!
